- TO:
- ALL COUNTY AND REGIONAL STAFF
- FROM:
- ALYSON CAMPBELL, DIRECTOR
- SUBJECT:
- MO HEALTHNET EX PARTE REVIEW REMINDER
- FORMS MANUAL ADDITION #11
DISCUSSION:
This memorandum is to remind staff the ex parte process is mandatory for all MO HealthNet levels of care and to introduce a new form the Report of Change/Need for Reassessment (IM-145 OTH). When an individual becomes ineligible at any MO HealthNet level of care, eligibility must be explored under every other MO HealthNet program where potential eligibility exists. This is called an Ex Parte Review. The ex parte review process was originally outlined in Income Maintenance memorandum IM-193 MC+/MEDICAID REV FMR#47 IM80PRE MR#31 FHC dated December 28, 2000.
Review the individual’s possible eligibility under all other MO HealthNet levels of care without the involvement of the participant. Use information from all available records such as Food Stamps, Child Care and Temporary Assistance, or data sources including SDX, BENDEX, IIVE, IMES, etc. When eligibility is established for another MO HealthNet program, register an application for the program and approve the participant for the new level of care with no break in MO HealthNet coverage. The individual should be moved to the best healthcare benefits package for which they qualify.
When other eligibility cannot be established from review of the available information, mail a Pre-Closing Notice (IM-80PRE) to the participant. This notice informs the participant of possible eligibility for other MO HealthNet programs and provides the participant the opportunity to contact the Family Support Division (FSD) to request evaluation for other eligibility. Send an Adverse Action Notice to the participant, when the participant does not respond within ten (10) day to the IM-80PRE.
If the participant responds to the FSD prior to the expiration date on the Adverse Action notice, void the adverse action to allow coverage to continue under the existing level of care until the determination is completed. If the participant reports possible eligibility for another MO HealthNet program after the Adverse Action Notice expires, the participant must complete an application for that program.
Prior to allowing a Pre-Closing Notice or Adverse Action Notice to expire, staff must:
- Review comments at the EUMEMROL screen for a FAMIS case or at the Client Contact tab/Notes folder of the head of household for a MEDES case.
- Complete a thorough search of the FSD Work Site for possible receipt of a written response from the participant during the Pre-Closing or Adverse Action Notice timeframes.
- Immediately register the new application and explore eligibility, when there is a comment in FAMIS or MEDES or information in the Work Site indicating that the participant has requested a review of benefits under another type of assistance.
NOTE: Following the ex parte review, if an individual is determined ineligible for any other program, take action to close the active case
In some instances, an override will be necessary to provide ongoing coverage while the application is pending. Requests for overrides will be sent through proper management channels to the following Program Development Specialists:
| • Kansas City Region – | Tisha Bowman Nathan Stamburski |
Tisha.Bowman@dss.mo.gov Nathan.Stamburski@dss.mo.gov |
| • Northeast Region – | Victoria Maney | Victoria.Maney@dss.mo.gov |
| • Northwest Region – | Elizabeth (Betsy) Friesz | Elizabeth.A.Friesz@dss.mo.gov |
| • St Louis Region – | Debra Murray | Debra.Murray@dss.mo.gov |
| • Southeast Region – | Melissa Wynn | Melissa.F.Wynn@dss.mo.gov |
| • Southwest Region – | Nathan Stamburski Tisha Bowman |
Nathan.Stamburski@dss.mo.gov Tisha.Bowman@dss.mo.gov |
The FSD is currently working in two distinct determination systems, the Family Assistance Management Information System (FAMIS), and the Missouri Eligibility Determination and Enrollment System (MEDES). The “Report of Change/Need for Reassessment” (IM-145 OTH) form was created to facilitate communications between FAMIS and MEDES offices to ensure that potential eligibility for other programs is explored.
When potential eligibility for another program is discovered or reported, the office receiving this information will register the application if they have the appropriate system access. When the participant should be closed in one system and made active in the other system, the office receiving the information should register the appropriate application, if they have access, and immediately complete the IM-145 OTH. If the receiving office is not able to register the application, check the appropriate box on the IM-145 OTH to document the application has not been registered. Then, scan the IM-145 OTH to the Work Site, indexing it as an application to the appropriate location to be processed in the other system.
EXAMPLE: Megan and her mother, Sally are currently active MO HealthNet for Families (MHF) in MEDES. Megan is turning age 19 on 11-05-xx and will no longer be age-eligible for MHF. There is documentation in the file that Megan is receiving Supplemental Security Income (SSI) benefits in the amount of $680 a month. Because Megan has a verified disability, the MEDES ES must register a FAMIS MO HealthNet for the Aged, Blind, or Disabled (MHABD) application for Megan. The Pre-Closing Notice and a new application form are not required. While the application will generate an alert on the FAMIS ALREMINDS (Alert/Reminders) screen, the MEDES ES must complete the IM-145 OTH and scan this form to the Work Site, to the appropriate location to be processed by a FAMIS office. The FAMIS and MEDES ES will coordinate communication to ensure that the MHF coverage continues pending the determination of the MHABD coverage, even if the determination continues after Megan’s 19th birthday.
NOTE: Because Sally was receiving MHF and removing Megan from her household will close Sally’s case, an Ex Parte review must also be completed to determine continued eligibility for Sally.
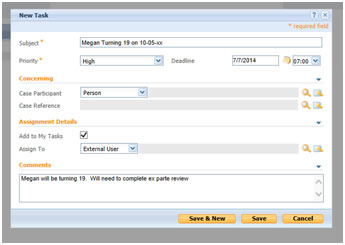
If a MEDES participant is approaching age one or age 19 within six months, the MEDES ES should set a task to conduct the ex parte review. If this task has already been set by another ES, duplication of the task is not necessary. Tasks may be set in the case or through the MEDES Home Page as in the example below:
During the Pre-Closing and Adverse Action Notice periods, the letters instruct the participant to contact the FSD Info Center to report possible eligibility such as pregnancy, blindness, or disability. A new script has been provided to the FSD Info Center, to ensure that this report is provided to the appropriate office as soon as possible so existing coverage can remain active while eligibility is determined for the newly requested program.
The FSD Info Center Script instructs staff to place a comment on the Eligibility Unit Member Role (EUMEMROL) screen for a FAMIS case or at the Client Contact tab, Notes folder for the head of the household on a MEDES case. The comment will capture the participant’s statement regarding the potential eligibility. After entering the comment, the FSD Info Center staff will send an email to the appropriate office informing FSD staff that the participant has requested a review for other eligibility. The email will include the name and Department Client Number (DCN) of the Head of Household (HOH), the name and DCN of the participant for whom a new determination is requested, and the type of assistance requested or the potential eligibility factor.
Management should continue to monitor Managed Reporting reports, Active Newborn Children Age 1 or Over and Family Medicaid Children Age 19 or Over, and ensure the ex parte review process is completed on any FAMIS Family MO HealthNet cases prior to closure. Refer to Income Maintenance memorandum IM-47 FAMIS FAMILY MEDICAL ASSISTANCE PROGRAM REPORTS ADDED TO MANAGED REPORTING SYSTEM, dated May 22, 2007 for further information regarding these reports. Refer to Income Maintenance memorandum IM-50 NEWBORN EX PARTE PROCESS AND PRE-CLOSING REVIEW (IM-80PRE) FORM REVISION for information on completing Newborn ex parte reviews.
Offices must develop a plan to complete ex parte reviews and requests for determination of appropriate levels of care in a timely manner. This plan must include processes for both FAMIS and MEDES cases until the transition to MEDES is complete.
NECESSARY ACTION:
- Review this memorandum with appropriate staff.
- The FSD Info Center must begin using the script provided.
- MEDES ES must immediately begin reviewing MEDES cases and establish ex parte review tasks for any participant turning age one or age 19 within six months of current actions if such task has not already been established by another ES.
- Local management must develop a plan to monitor and process ex parte reviews to avoid lapses in coverage.
ATTACHMENTS:
AC/ns/mks/df