- TO:
- ALL COUNTY AND REGIONAL STAFF
- FROM:
- ALYSON CAMPBELL, DIRECTOR
- SUBJECT:
- ACTIVE MEDES CASES IDENTIFIED AT REPORTED CHANGE AS ELIGIBLE TRANSITIONAL MO HEALTHNET
- FORMS MANUAL REVISION #12
DISCUSSION:
The purpose of this memorandum is to:
- Instruct staff to manually track Missouri Enrollment and Eligibility Determination System (MEDES) MO HealthNet for Families (MHF) participants who, due to a change, are now eligible for Transitional MO HealthNet (TMH); and
- Provide instructions on manually generating and processing TMH quarterly reports.
MEDES does not currently support TMH functionality. Until this functionality is present, the following instructions must be followed to manually process TMH for active MHF MEDES cases. All TMH eligibility criteria must be met. Until the MEDES manual is updated use the criteria found in Income Maintenance (IM) Manual section 0910.000.00 TRANSITIONAL MEDICAL ASSISTANCE (TMA). Review MXIX to confirm MHF eligibility for three (3) of the last six (6) months.
This memo includes:
- Instructions for Processing TMH in MEDES
- The Quarterly Reports are Received Timely
- The First Quarterly Report is Not Received or is Incomplete
- The Second or Third Quarterly Report is Not Received or is Incomplete
- The First Quarterly Report is Received Late
- The Second or Third Quarterly Report is Received Late
- TMH Expires at Twelve Months
Instructions for Processing TMH in MEDES
When an active MHF household reports a change that will move the household to TMH from MHF, follow these steps for processing quarterly reports:
- Active participants must be left at MHF level of care in MEDES.
- Enter an income amount of one dollar ($1) monthly, and put the actual income amount in the Notes section of the Income Evidence;
- Send a manual IM-80 TMH to the participant notifying them of the transition to TMH and the requirement to return quarterly reports timely.
- Eligibility Specialists (ES) must manually send the quarterly reports as follows:
- The first (1st) Transitional MO HealthNet Quarterly Report form IM-55A, must be mailed within the first 10 days of the third month of TMH eligibility. This form must be returned by the 21st day of the fourth month;
- The second (2nd) Transitional MO HealthNet Quarterly Report form IM-55B, must be mailed within the first 10 days of the sixth month of TMH eligibility. This form must be returned by the 21st day of the seventh month; and
- The third (3rd) Transitional MO HealthNet Quarterly Report form IM-55C, must be within the first 10 days of the ninth month of TMH eligibility. This form must be returned by the 21st day of the tenth month.
This information is found in the IM Manual section 0910.025.00 Quarterly Report Requirements.
- The assigned ES must manually track when the reports are due. The ES must review ITrack RS and the FSD Work Site for receipt of the quarterly reports.
- The ES must document when quarterly reports are sent to the household by adding a note to the Head of Household (HOH) Person Page:
Subject: TMH Quarterly Report # (enter the number of the report)
Note: TMH quarterly report ## was mailed on 08/01/yyyy and is due by 09/21/yyyy. The IM-55A has been scanned to the virtual file room.
The Quarterly Reports are Received Timely
When the quarterly reports are received timely:
- The ES must review the report for completeness and determine if the household continues to be TMH eligible. Refer to IM Manual sections 0910.015.00 ELIGIBILITY DURING FIRST SIX MONTHS (TMH) and 0910.020.00 ELIGIBILITY DURING THE SECOND SIX MONTH PERIOD (TMH).
- The ES must enter a note into MEDES on the HOH Person Page.
Subject: Quarterly Report # (enter the report number) received.
Note: TMH quarterly report ## was received on mm/dd/yyyy. The report was completed and signed by the participant. The household remains TMH eligible. - A new task must be sent by the ES to mail the next quarterly report.
The First Quarterly Report is Not Received or is Incomplete
After the ES has reviewed ITrack RS and the FSD Work Site and determined that the quarterly report has not been received, or an incomplete report is received:
- Within the first 5 days of the sixth month, the ES must complete an Ex Parte review and if necessary, send a manual IM-80PRE informing the household that TMH is ending due to the quarterly report not being received, or that the quarterly report was incomplete. Refer to Income Maintenance memorandum IM-63 MO HEALTHNET EX PARTE REVIEW REMINDER.
- Once the IM-80PRE has expired the ES must review all comments and data sources to determine if participant has responded to the IM-80PRE. If the participant has not responded, the Income Evidence must be updated and an IM-80TMH must be sent. The Income Evidence change is made by updating the received date and effective date to the expiration date of the IM-80TMH. The income amount will also be updated to reflect the amount initially reported which caused ineligibility for MHF. This evidence must be applied to the Integrated Case (IC).
NOTE: If the ES discovers a subsequent change in income for the household, the new amount must be entered and verified instead of the amount shown in the Income Evidence note.
- The Product Delivery Case (PDC) Determinations Tab must be viewed by the ES to ensure the coverage change for the household is correct.
- The ES must enter a note on the HOH Person Page explaining the:
- First quarterly report was not received or was incomplete.
- Task they have set to complete the ex parte review, and
- Outcome of the ex parte review.
The Second or Third Quarterly Report is Not Received or is Incomplete
After the ES has reviewed ITrack RS and the FSD Work Site and determined that the quarterly report has not been received, or an incomplete report is received:
- If the second or third quarterly report is not received timely, the adults in the household must be suspended from coverage at payroll closing (payroll closing is the 4th Friday of a month unless the last day of the month falls on Monday, in this case, payroll closing is the 3rd Friday of the month).
NOTE: An IM-80 is not required as the adults are merely being suspended.
- An Ex Parte review of all comments, data sources and the record must be completed prior to suspending adults in the household in order to determine if they are eligible for other MO HealthNet coverage.
- If the Ex Parte results in the adults moving to another MO HealthNet category, send an IM-33MHF to notify them that the coverage has changed. If the Ex Parte review does not result in eligibility for another MO HealthNet category, send the household an IM-58 Transitional MO HealthNet Suspension Notice advising them that the adults in the household are suspended for failure to return the second or third quarterly report.
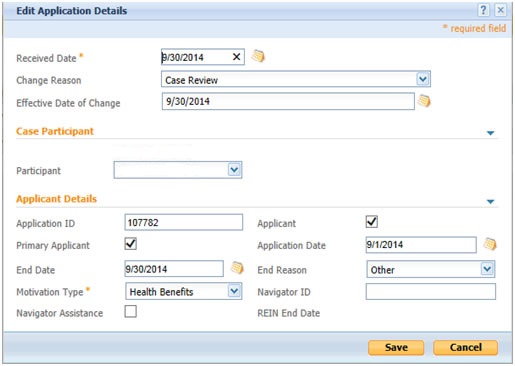
- To suspend the adults the Application Details Evidence must be updated. The Received date, Effective Date of Change, and End Date must be the last day of the month in which TMH is to end. The end reason of “Other” must be entered (see example below). Save this evidence and then apply it to the IC.
The ES must enter a note on the HOH Person Page explaining why the parent(s) TMH coverage has been suspended.
The First Quarterly Report is Received Late
If the first quarterly report is received late review IM Manual section 0910.025.10 Good Cause For Failure To Return Quarterly Report (TMA):
- If good cause is allowed, reinstate TMH coverage by updating the Income Evidence to show an Amount of $1. Save this change and apply it to the IC. Review the PDC Determinations Tab to ensure that coverage is reinstated to the family. The ES must enter a note on the HOH Person Page explaining why good cause was allowed.
- If good cause is not allowed the ES must enter a note on the HOH Person Page explaining why.
NOTE: If the household contacts the Family Support Division (FSD) indicating possible eligibility due to disability, pregnancy, blindness or change in circumstances, restore eligibility to TMH pending an eligibility determination under the appropriate category of assistance. Reinstate the person(s) indicating possible eligibility using the emergency spreadsheet process .
The Second or Third Quarterly Report is Received Late
Upon receipt of the second or third quarterly report suspended TMH adults must be reinstated. Review IM Manual section 0910.025.10 Good Cause For Failure To Return Quarterly Report (TMA) for the household:
- If good cause is allowed reinstate coverage back to the date of suspension by editing the Application Details evidence. The Received Date and Effective Date of Change must be updated to the current date and the End Date must be removed along with the End Reason. Apply the changes to the IC and review the PDC determinations tab to ensure coverage is showing correctly for the adults.
- If good cause is not allowed reinstate effective the first of the month following the receipt of the report by utilizing the emergency spreadsheet process. Staff must review MXIX the following day to ensure that coverage is showing correctly.
- The ES must enter a note on the HOH person page explaining why good cause was allowed or not allowed, and the ES must state when coverage has been reinstated for the parent(s).
TMH Expires at Twelve Months
The ES must set a task for the first day of the twelfth month of TMH:
- Explore the household’s eligibility for other MO HealthNet categories by completing an Ex Parte review.
- Use the information from the last quarterly report to evaluate eligibility. The Income Evidence must be updated within the first ten days of the twelfth month. Update the Received Date and Effective Date of Change to the first day after the expiration of TMH. Update the Income Amount to reflect the most recent income information received. The Income evidence must be applied to the Integrated Case (IC).
- The PDC Determinations Tab must be viewed by the ES to ensure the coverage change for each individual household member is correct. If appropriate, send a manual adverse action notice.
- Review the MEDES notice and MXIX to insure that the participant’s benefits are correct based on the outcome of the review.
- The ES must enter a note on the HOH Person Page explaining the outcome of the ex parte review.
NECESSARY ACTION:
- Review this memorandum with appropriate staff.
- Follow this manual process until TMH functionality is present in MEDES.
ATTACHMENTS:
- IM-33MHF Action Notice
- IM-55A First Transitional MO HealthNet Quarterly Report
- IM-55B Second Transitional MO HealthNet Quarterly Report
- IM-55C Third Transitional MO HealthNet Quarterly Report
- IM-58 Transitional MO HealthNet Suspension Notice
- IM-80TMH Adverse Action Notice
AC/ns/mks/df