FROM: KIM EVANS, DIRECTOR
SUBJECT: COVID-19 ECONOMIC IMPACT PAYMENTS RESULTING FROM THE CORONAVIRUS AID, RELIEF, AND ECONOMIC SECURITY (CARES) ACT FOR THE MO HEALTHNET, FOOD STAMP, TEMPORARY ASSISTANCE AND CHILD CARE SUBSIDY PROGRAMS
MANUAL REVISION #15
MO HealthNet 0805.015.10 1025.015.01.02
Food Stamps 1110.020.30 1115.015.90
Temporary Assistance 0205.005.30.10 0210.015.35.40
DISCUSSION:
Economic Impact Payments (EIP), also known as Stimulus Payments, were approved as part of the CARES Act which was signed into law on March 27, 2020. This act contains changes that affect the Food Stamp (FS, also known as SNAP) Program, Temporary Assistance (TA) Program, Child Care Subsidy (CC), and MO HealthNet (MHN) Programs.
Economic Impact Payments
U.S citizens and resident aliens will receive the EIP of $1,200 for individual or head of household filers, and $2,400 for married filing jointly if:
- they are not a dependent of another taxpayer and
- have a work eligible Social Security number with Adjusted Gross Income (AGI) up to:
- $75,000 for individuals
- $112,500 for head of household filers and
- $150,000 for married couples filing joint returns
Taxpayers will receive a reduced payment if their AGI is between:
- $75,000 and $99,000 if their filing status was single or married filing separately
- $112,500 and $136,500 for head of household
- $150,000 and $198,000 if their filing status was married filing jointly
The amount of the reduced payment will be based upon the taxpayers specific AGI.
Eligible retirees and recipients of Social Security, Railroad Retirement, Disability or Veterans’ benefits as well as taxpayers who do not make enough money to normally have to file a tax return will receive a payment. This also includes those who have no income, as well as those whose income comes entirely from certain benefit programs, such as Supplemental Security Income benefits.
Retirees who receive either Social Security Retirement or Railroad Retirement benefits will also receive payments automatically.
MO HealthNet Non-MAGI Programs, Food Stamps (FS/SNAP), Temporary Assistance (TA), and Child Care Subsidy (CC)
- Payments are excluded as income.
- Payments are excluded as a resource for the first 12 months from receipt.
NOTE: EIP payments reported in the month received will be entered as a resource. DO NOT enter as income in FAMIS. Any money left from the EIP 12 months after receipt will be counted as a resource.
MO HealthNet for Families (MAGI) Programs
- Payments are excluded as income.
NOTE: Make a comment on the case of the amount received. The payment is not to be entered into income on case.
- Example of note comment: Smith reported she received $1700.00 from the Economic Stimulus Payment on 4/16/2020.
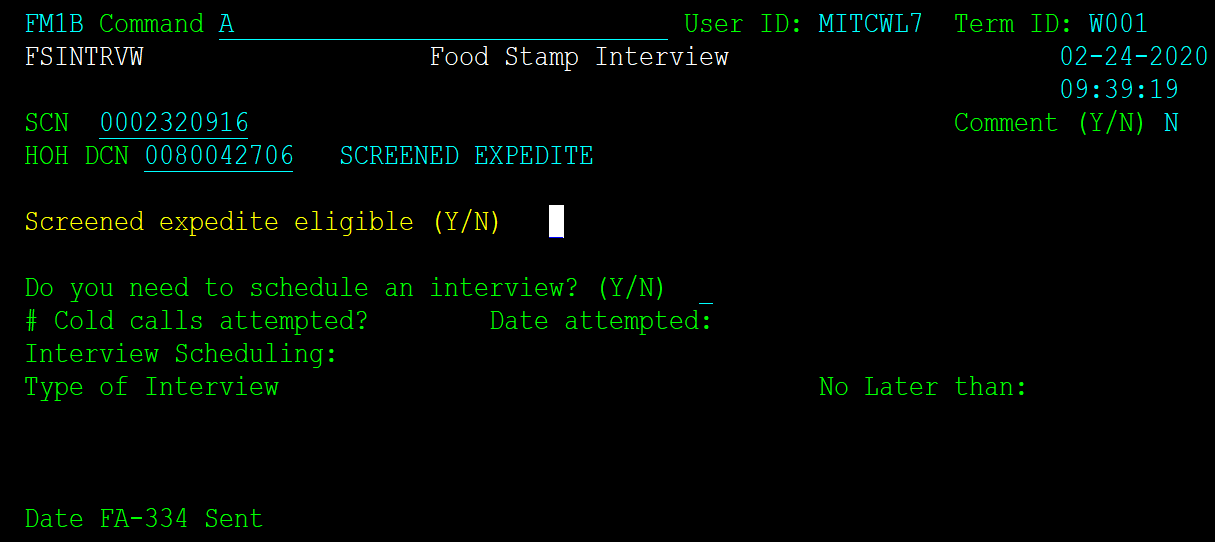
FAMIS Entries
If the EIP is reported as income in the month received, enter it as a resource on the SELFRES (FMWB) screen. DO NOT ENTER AS INCOME ON SELINC (FMX2). Refer to the examples below for guidance to capture the EIP income as an excluded resource. The excluded amount should always equal the total EIP when entering for the same month it was received along with any other excluded balances for that month. Use Code CV in the Excl Rsn field for the Economic Impact Payment or CB if multiple exclusion reasons exist. Please use the Verification Matrix for acceptable verification codes.
If the balance of the EIP is reported the month after receipt exclude any remaining balance of the EIP in the accounts as CV following normal procedures in entering liquid resources.
No Resources and received the EIP
To capture the full amount of the EIP you need to enter the full amount as Cash since they did not deposit it in an account.
|
|
Income
|
Checking
|
Savings
|
Cash
|
Excluded
|
|
Reported
|
$1200 EIP
|
none
|
none
|
none
|
$1200 EIP
|
|
FAMIS entry
|
No entry
|
No entry
|
No entry
|
$1200 excl (-) $1200 (CV) = $0 counted
|
Resource More than EIP
For a case that has deposited the full EIP only exclude up to the EIP amount, leaving the remainder to be counted.
|
|
Income
|
Checking
|
Savings
|
Cash
|
Excluded
|
|
Reported
|
$1200 EIP
|
$1500
|
none
|
none
|
$1200 EIP
|
|
FAMIS entry
|
No entry
|
$1500 excl (-) $1200 (CV) = $300 counted
|
No entry
|
No entry
|
Resource Less than EIP
For a case that has split the deposit of the EIP but did not deposit the full amount, enter the remainder as cash.
|
|
Income
|
Checking
|
Savings
|
Cash
|
Excluded
|
|
Reported
|
$1200 EIP
|
$800 Balance
|
$200 Balance
|
none
|
$800
$200
$200
= $1200 EIP
|
|
FAMIS entry
|
No entry
|
$800 excl (-) $800 (CV) = $0 counted
|
$200 excl (-) $200 (CV) = $0 counted
|
$200 excl (-) $200 (CV) = $0 counted
|
Resources More than EIP and Other Current Income
For reports of EIP income and other income which would be excluded and both were deposited into an account, exclude the total of both the EIP and the Current Income amounts.
|
|
Income
|
Checking
|
Savings
|
Cash
|
Excluded
|
|
Reported
|
$1200 EIP
$800 Other Income
|
$2100
|
none
|
none
|
Make comment on $800 Current Income and that $1200 was from EIP
|
|
FAMIS entry
|
$800 Other Income
|
$2100 excl (-) $2000 (CB) = $100 counted
|
No entry
|
No entry
|
Resources Less than EIP and Other Current Income
For reports of EIP income and other income which would be excluded but is less than the reported balance in their accounts, enter the remainder of the EIP only as Cash.
|
|
Income
|
Checking
|
Savings
|
Cash
|
Excluded
|
|
Reported
|
$1200 EIP $800 Other income
|
$700
|
$200
|
none
|
Make comment on checking that this was from Current income. Savings comment would reflect that $100 was from Current Income and that $100 was from EIP.
|
|
FAMIS entry
|
$800 Other Income
|
$700 excl (-) $700 (CI) = $0 counted
|
$200 excl (-) (CB) = $0 counted
|
$1100 excl (-) $1100 (CV) = $0 counted
|
IRS Coronavirus Economic Impact Payment Information
26 U.S. Code 6409
NECESSARY ACTION:
- Review this memorandum with appropriate staff.
KE/nw/ph/rw