FROM: KIM EVANS, DIRECTOR
SUBJECT: CHANGES TO THE SUPPLEMENTAL NUTRITION ASSISTANCE PROGRAM (SNAP) ABLE-BODIED ADULTS WITHOUT DEPENDENTS (ABAWD) AGE LIMIT AND EXEMPTIONS
MANUAL REVISION #
DISCUSSION:
The Fiscal Responsibility Act (FRA) of 2023 adds three new exemptions to the ABAWD Work Requirement and gradually increases the upper age limit from 49 years old to 54 years old. These changes are effective 9/1/2023.
New Exemptions
Three new Employment Assessment coding options have been created for the new exemptions:
- 40—Aged out of Foster Care, Under 25 years old:
- This exemption is for an applicant/participant who is 24 or younger and aged out of the foster care system of any state, district, territory, or tribal organization at age 18 or older.
- Verification is required.
Note: Exemption will be automatically ended, coding changed to non-exempt (code 22), and non-work months added (if applicable) when participant turns 25 years old.
- 41—Veteran:
- This exemption is for any participant who served in any branch of the United States Armed Forces, including Reserves/Guard, regardless of the conditions of their discharge or release.
- Verification is required.
- 42—Homeless:
- There has been no change to the definition of homeless. Refer to 1100.010.00 Definitions
- Status code: EXE
- Verification is not required.
Note: Code 15 is no longer to be used for homelessness. All participants currently coded 15 will be updated to 42. Coding will need to be reassessed at next mid-certification review, recertification, or reported change.
When a household member is eligible for more than one exemption, staff must select the exemption that is most beneficial to the participant for the duration of certification.
New Employment Assessment Statuses
In order to allow for verification to be requested and for the participant to be exempted from ABAWD requirements but still referred to SkillUP, two new statuses were created for use with the Aged Out of Foster Care and Veteran exemptions:
- AEX – ABAWD-Only Exemption
- PEN – Pending Assessment
- Pends the case for verification
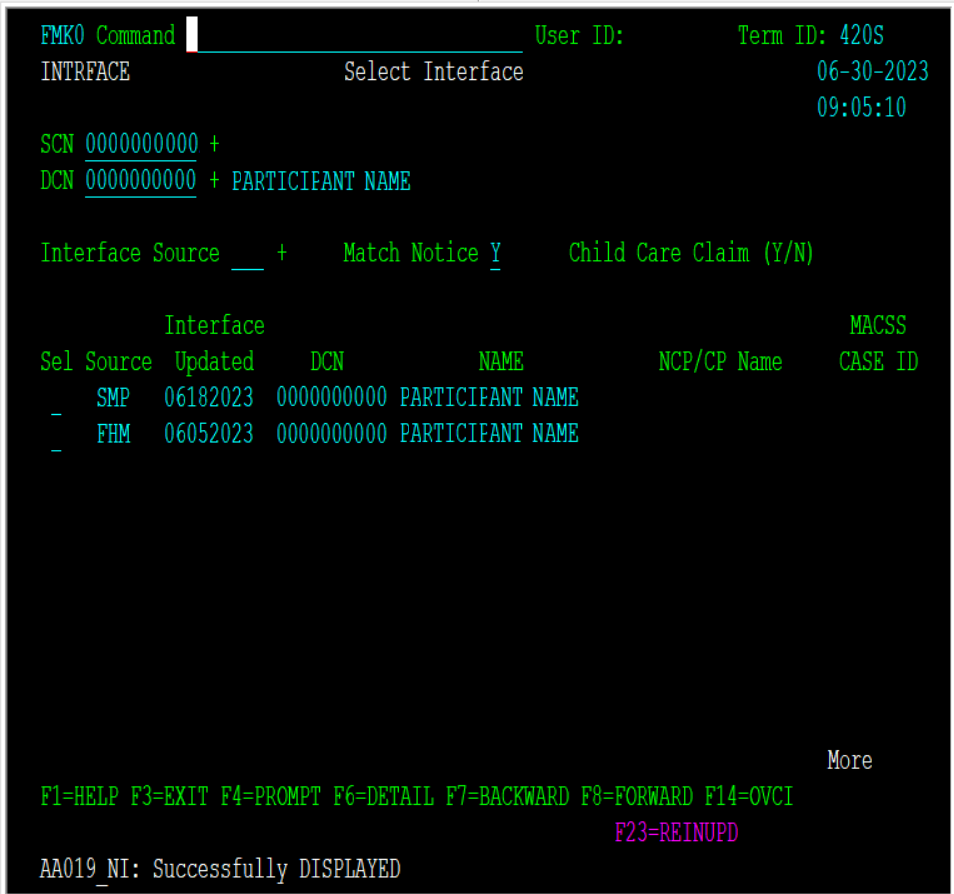
Once verified, eligibility for the Foster Care or Veteran exemption does not need to be re-verified for subsequent applications or recertifications. When verification is received and the status updated to AEX, a comment must be entered on the Employment Assessment (EMPLOY/FMMS) screen to document how the exemption was verified.
Note: If verification is not provided then the eligibility system will update the coding to non-exempt (code 22) and, if applicable, either add non-work months or reject the member if they have already used their 3 non-work months.
- If a SkillUP exemption applies then a case should not be pended for verification on an ABAWD-only exemption.
Age Limit Increases
The age limit for the ABAWD work requirement will increase as follows:
- 18 – 50 years of age, effective 9/1/2023
- 18 – 52 years of age, effective 10/1/2023
- 18 – 54 years of age, effective 10/1/2024
The age limit increases apply at application/recertification, mid-certification review, and when adding a household member. Non-work months will not be automatically added for active participants. A participant’s work assessment code must be reviewed at every mid-certification review, recertification, or when the participant reports work activities or an exemption.
SNAP Manual Revisions
Updates were made to the manual sections listed in the Manual Revision section of this memo to remove references to the ABAWD age range, update links to re-named sections, update formatting, and to reflect current policy, procedures and terminology.
Additional updates were made to the manual sections below:
ABAWD Policy Updated:
Title Changes
System generated forms and notices have been updated to reflect these changes.
NECESSARY ACTION:
- Review this memorandum with appropriate staff.
KE/mn